Public Health Sudbury & Districts and the COVID-19 pandemic: From risk to recovery and resilience (February 2022)
PDF version (2 MB, PDF)
It has been nearly two years since the first case of COVID-19 infection was confirmed in the Sudbury and Manitoulin districts. During this time, Public Health Sudbury & Districts (Public Health) has provided leadership and essential services to manage the pandemic and guide communities to best protect themselves during an unprecedented and ever-changing crisis.
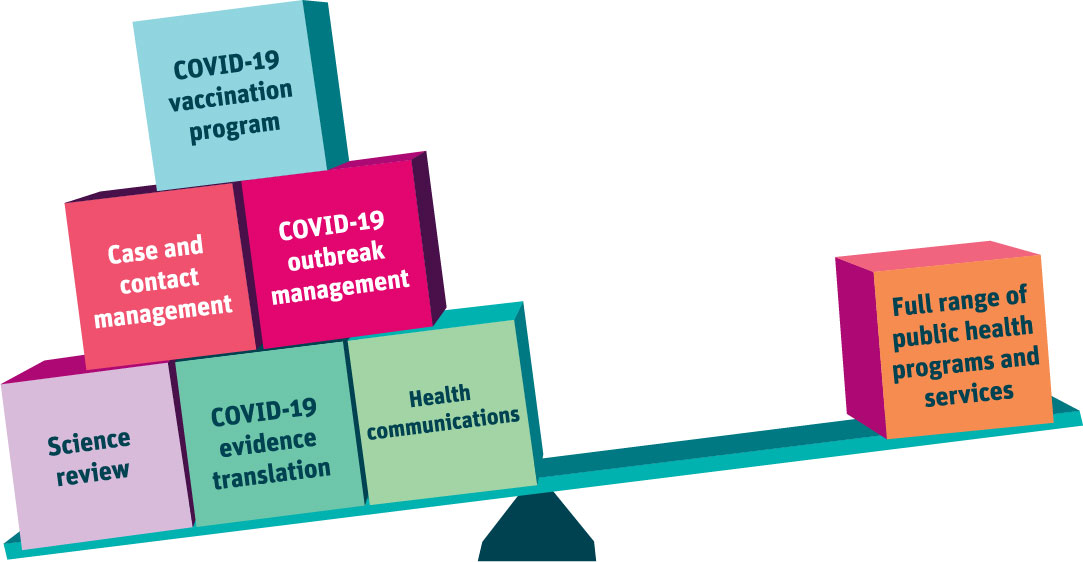
Public Health has worked to understand, translate, and action the best available evidence, including extensive and ongoing reviews of science and local epidemiology. All these extraordinary efforts have been vital. They have also come at great opportunity costs. Public Health has had to stop or radically reduce many of its other public health programs and services during this two-year period, creating a growing backlog of services and unmet needs.
While the pandemic continues to demand Public Health leadership and resources, we are actively looking forward to planning for the future. We are investing energy in planning now so that we are ready to assess and address ongoing and emerging health needs that require public health intervention. We are an active partner in the local recovery endeavour—creating and contributing to post-pandemic strong and resilient communities.
Public Health’s response to the COVID-19 pandemic
Public health has been critical to the province of Ontario’s pandemic response. Locally, Public Health has led case, contact, and outbreak management, the vaccination program, behaviour change initiatives, and local protective measures. Beneath the surface has been the essential work of data analysis and epidemiological reviews, communications and stakeholder engagement, human resources, and information technology supports.
In working with many partners, we have kept our eye on the collective goal of protecting health and the health system, and of keeping critical infrastructure and services operating. There has been no roadmap—but we have charted a path together. Now, as immunity grows with increasing vaccination rates and successive waves of new variants, we look forward to turning the corner and assessing and addressing the impact of the COVID-19 pandemic on the overall health of our communities and contributing to our collective recovery.
Public Health’s COVID-19 response efforts by the numbers (up to January 31, 2022)
- 9 340 total COVID-19 cases
- 22 007 contacts identified and followed
- 227 outbreaks
- 1 992 vaccination events
- 173 149 people received their first dose
- 169 169 fully vaccinated
- 91 827 people received their third dose
- 1 058 people received their fourth dose
- 435 203 total doses administered
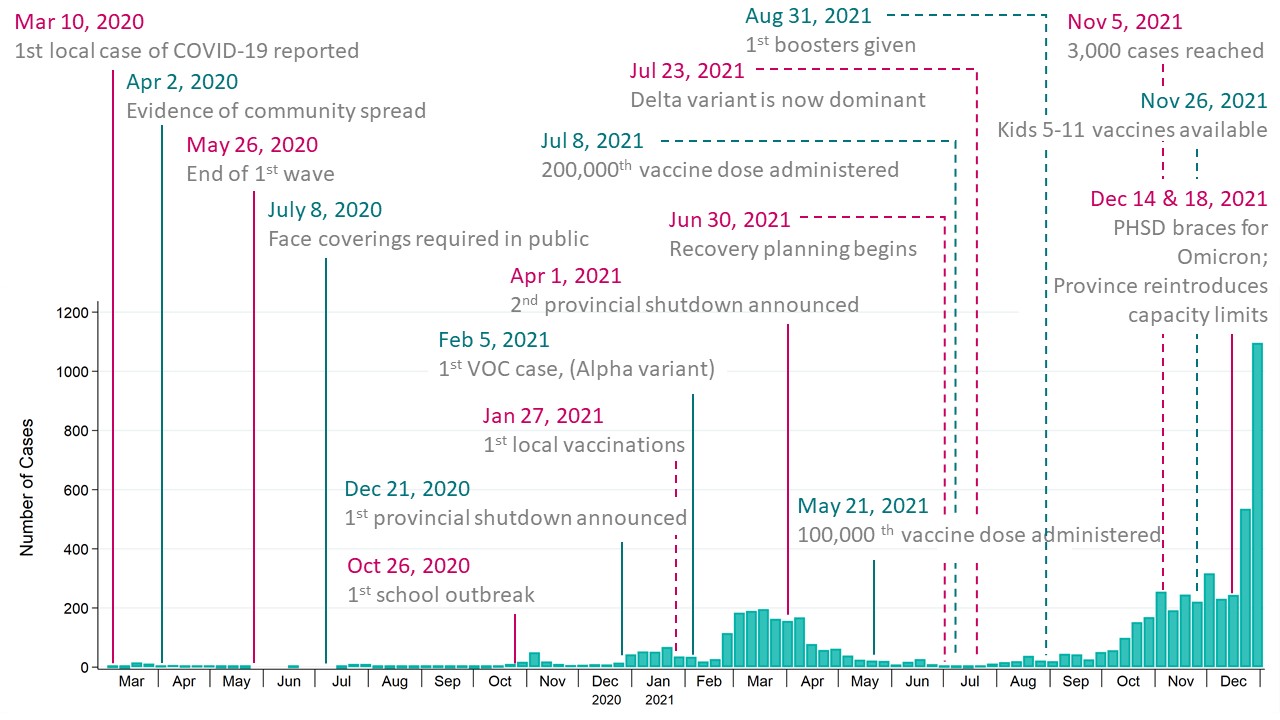
Figure 1: Key milestones of the COVID-19 pandemic in the Sudbury and Manitoulin districts service area from March 1, 2020, and December 31, 2021
The COVID-19 journey to date has not been straight-forward (Figure 1). We have experienced successes and setbacks and, as elsewhere, we are currently in the midst of another COVID-19 wave (Omicron B.1.1.529 variant). We are fortunate that although the mutations in the Omicron variant have made it more transmissible, they have not made it more severe. Unfortunately, due to the high number of infections, there will still be an increase in the number of people with serious disease requiring hospitalization.
The characteristics of the Omicron variant have required changes in provincial guidance. As a result, intensive public health efforts must be directed to protect high-risk settings such as long-term care homes and group homes, to protect the most vulnerable. Case, contact, and outbreak management focused on these high-risk settings will continue, as will ongoing vaccination efforts to ensure Ontarians are fully vaccinated and boosted. Although Omicron can more readily infect those who are immune from vaccine or previous infection, three doses of vaccine remain very protective against serious disease and hospitalization1,2. This transition is difficult—but it is yet another adaptation required by an ever-changing virus and, collectively, we will champion this change too.
Public Health’s transition to recovery while the pandemic continues its path will require the careful management of competing pressures. We have to balance responding to the pandemic through vaccination and case, contact, and outbreak management with investing in recovering from the pandemic through reinstating public health programs and services to assess and address ongoing and emerging health needs in the wake of the pandemic.
Recovery and resilience: Reducing Public Health’s backlog and building back better
As we have learned more and throughout each wave of the COVID-19 pandemic, the collective response has had to adapt many times to best protect individuals and our communities from the virus. From all walks of life—municipalities, health care providers, volunteer groups, local businesses, private citizens—everyone has contributed to the success of the local COVID-19 response. Public Health has been humbled by the contribution and commitment of so many as we lead our own responsibilities in this public health emergency.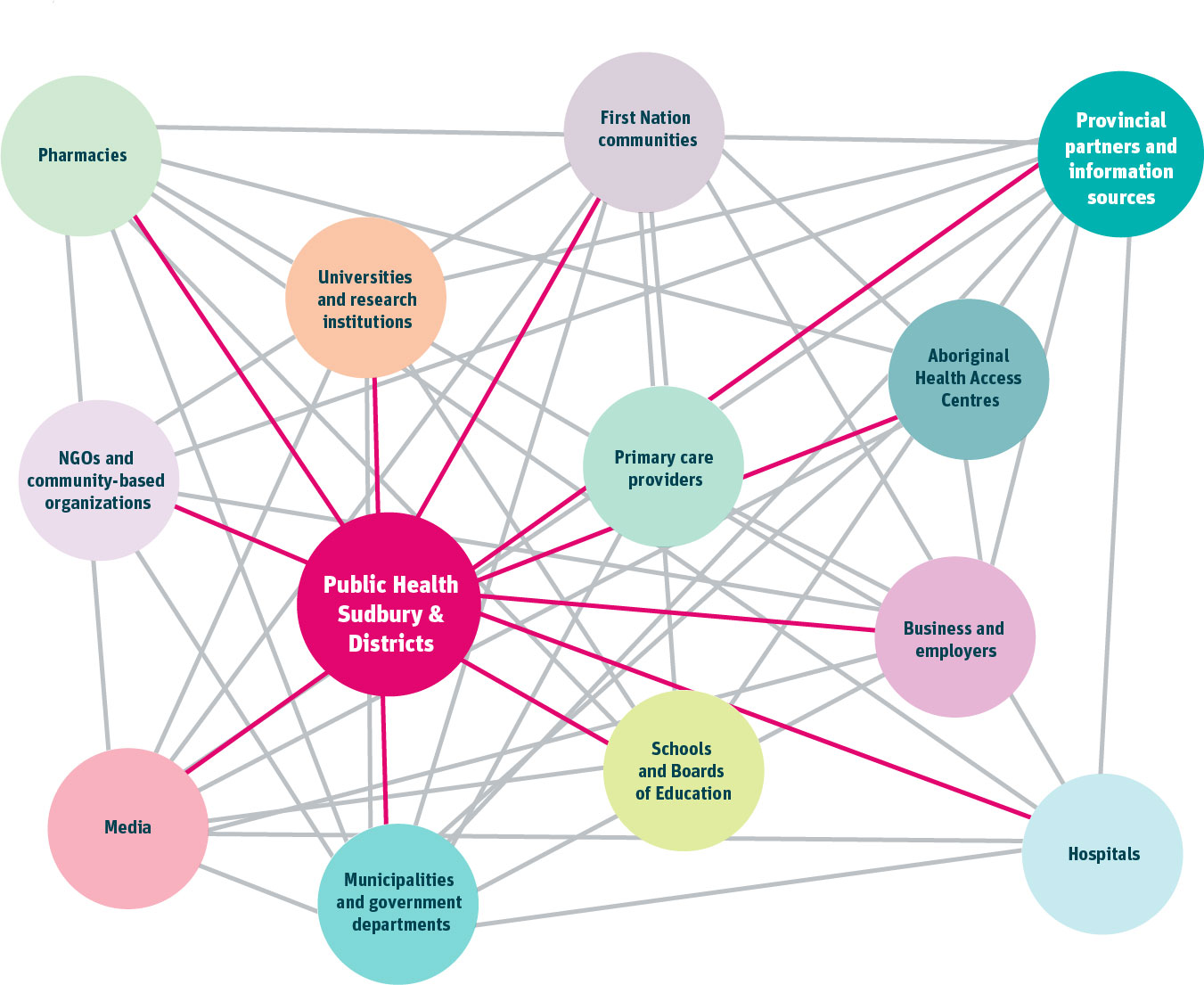
Adverse impacts of COVID-19 and the COVID-19 response
The effects of the pandemic have not been experienced in the same way by all. Those experiencing systemic barriers to health and well-being prior to the COVID-19 pandemic continue to face disproportionate impacts during the pandemic, exacerbating underlying health inequities3,4.
Further, individuals who are more marginalized—socially, economically, culturally, racially—have borne a heavier burden both in terms of actual infection rates and in the burden of the pandemic control measures themselves. This includes, for example, isolation, job loss, loss of income, mental health, community connections, cultural ceremony, and stigma. The risks of the pandemic and pandemic control measures have been different for different groups such as individuals who are older, those living with chronic conditions, people with disabilities, and those who are living in poverty or with unstable employment.
Understanding the adverse impacts of the pandemic and how they are experienced unevenly across our communities is critical to informing how public health can contribute to recovery for all. The public health mandate includes the requirement to reduce inequities in health and support opportunities for health for all. This particularly includes those experiencing greater disadvantage due to structures and systems beyond individual control. This work involves a variety of actions that target “upstream” and “downstream” determinants of health (Figure 2). Examples of upstream and downstream programs and services delivered by Public Health are overlaid on Figure 2.
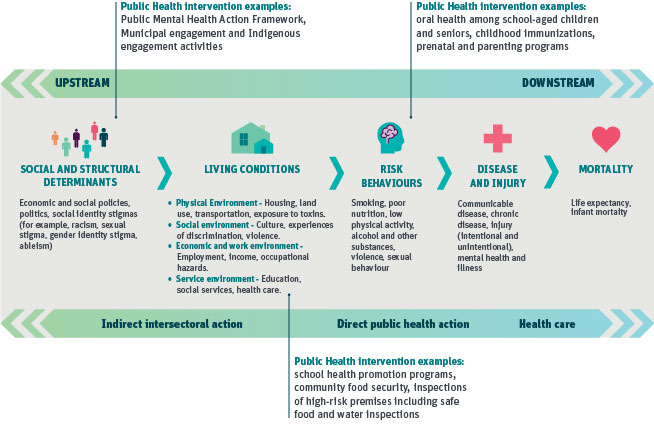
Figure 2: Continuum of interventions to address the determinants of health © All rights reserved. Chief Public Health Officer’s Report on the State of Public Health in Canada: A Vision to Transform Canada’s Public Health System. Public Health Agency of Canada. Modified, adapted and reproduced with permission from the Minister of Health, 2021.
Impacts of the COVID-19 pandemic on public health capacity
The prolonged and intense response to the COVID-19 pandemic has had significant repercussions for Public Health capacity. This includes direct impacts on our programs and services and on our workforce.
According to a recent survey of local public health units in Ontario, respondents reported reduced capacity to meet the requirements for the mandated programs and services outlined in the Ontario Public Health Standards5 as a result of the redeployment of local public health staff to COVID-19 response activities6. For example, of the required programs and services outlined in the Foundational Standards, public health was only able to complete 17% of population health assessment, 26% of health equity, and 30% of effective public health practice programs and services, on average, between the start of the pandemic (March 2020) and August 30, 2021. A similar pattern was observed for the completion of the requirements under the 13 Program Standards6. While a small proportion of the mandated expectations were completed, most of the work was linked in some way to COVID-19 response efforts. Much of the work suspended altogether were health promotion-related programs and services6.
Locally, responding to the pandemic has required the redeployment of approximately 75% of Public Health Sudbury & Districts staff to COVID-19 response efforts over the course of two years. This is in addition to the temporary hiring of additional staff and our reach out to other public health units and the provincial workforce for support at various points in the pandemic. The obvious consequence has been the suspension or radical reduction for two years of all non-COVID-19 related public health programs required under the Ontario Public Health Standards.
The public health workforce is comprised of multi-disciplinary staff including:
- nurses,
- public health inspectors,
- health promoters,
- epidemiologists,
- registered dietitians, and
- dental hygienists and educators among others.
For Public Health Sudbury & Districts, the pandemic response has required that these various staff adjust to unfamiliar pandemic work, not normally part of their roles. The many readjustments, relentless intensity and long hours of work, combined with the uncertainty everyone has experienced in the pandemic, have left our workforce vulnerable and at risk. Public Health staff have demonstrated incredible resiliency and commitment to serving the communities in the Sudbury and Manitoulin districts. However, Public Health’s contribution to the path to recovery must take into consideration the well-being of staff and ensure opportunities for their own recovery—investment in our human capital is critical.
Addressing the backlog: Public Health priorities for recovery programming
As Public Health begins to plan for its role in the local recovery endeavour, we have identified initial priorities for public health action. The priorities are based on our assessment of health impacts observed to date, combined with our knowledge of community strengths to be leveraged and gaps to be bridged. Guided by our organizational values of trust, humility, and respect, Public Health has further considered initial feedback from local partners—knowing there is further engagement to be undertaken.
While the priorities will continue to be reassessed as we navigate future developments of the pandemic, Public Health’s recovery priorities align with priorities identified through a provincial survey of local public health agencies in Ontario6. Results from this survey indicated that over 90% of respondents identified mental health promotion, substance use and harm reduction, and child immunization catch-up in their top priorities for recovery, with food safety inspection and oral health rounding out the top five.
Consensus on the top priorities for recovery was informed by the common experience of local public health units’ reduced capacity to meet the requirements of the Ontario Public Health Standards. For example:
- according to 16 local public health units, less than 1% of eligible children received oral health screening in schools in the 2020-2021 school year, compared to the 2019-2020 school year6 .
- services provided as part of the Healthy Babies Healthy Children program—a program targeting vulnerable mothers and infants—was also greatly impacted. While many local public health units transitioned to online and virtual delivery, the uptake of services using this method of delivery was low among this population. According to 17 local health units, less than 10% of Healthy Babies Healthy Children families received virtual ‘home visits’6.
These are but two examples of public health programs and services that have a growing backlog in Ontario. The long horizon and preventive nature of much of public health work means that the impact of these service disruptions will not be known for some time. What is anticipated, however, is that the impacts will again be unevenly experienced, as many public health programs and services are designed to “level up” and preferentially support those experiencing the most disadvantage.
Public Health Sudbury & Districts’ four recovery priorities include a focus on actions that will have the greatest impact for individuals and groups facing the highest disadvantage and fewest opportunities for health. The priorities bring us back to the core business of public health and the mandate to level up and create healthier communities for all.
Getting children back on track.
This includes:
- Oral health among school-aged children
- Healthy Babies Healthy Children programming including healthy eating supports
- Prenatal and parenting programs, services, and supports
- Children’s mental health and resiliency
- Childhood immunizations and other vaccine-preventable diseases
- School health promotion including the Northern Fruit and Vegetable Program
Levelling up opportunities for health.
This includes:
- Health equity and racial equity programs, services, and supports including allyship training
- Sustainable food systems and food security
- Municipal engagement and Indigenous engagement activities
- Senior’s health including dental health services and Stay on Your Feet programming
Fostering mental health gains.
This includes:
- Public Mental Health Action Framework including anti-stigma initiatives
- Internal mental health literacy competencies and supports targeting Public Health staff
- Community Drug Strategy collaboration and prevention programs
- Eating disorders prevention, promotion, and early interventions
- Healthy behaviours, supportive environments, movement, and physical activity
Supporting safe spaces.
This includes:
- Healthy built and natural environments including health hazards prevention and mitigation
- Inspections of high-risk premises including safe food and water inspections
- Routine inspections of childcare facilities
- Community Drug Strategy, including the Needle Exchange Program
- Infectious and communicable disease prevention & control programs and services
- Sexual health programs and services
Next steps: Planning for priority Public Health programs in 2022
There are significant intersections between the four Public Health recovery priorities. This will assist in amplifying our actions as we collaborate across the agency to plan concrete programs and services. Given that Public Health’s transition to recovery is occurring concurrently with the need for ongoing pandemic response, our approach is streamlined so that it is adaptable to these competing needs as they evolve.
The challenge of Omicron
Omicron is now the dominant strain in Ontario and is currently our biggest threat and challenge to resuming the full breadth of public health programs and services. It is estimated that each Omicron case is infecting 4.5 times more individuals than the Delta variant. We must use the tools in our toolbox to overcome this challenge, which includes vaccines. For Omicron, having three doses of the COVID-19 vaccine, compared to two, offers significantly more protection against severe illness and hospitalization2. While our actions and recommendations are based on the best available evidence, we also don’t know if new variants will emerge in the future. Public Health recognizes the toll the pandemic has and continues to take on everyone, but we must hold steadfast to these COVID-19-safe measures. We will continue to provide timely and transparent updates to the community; we ask you to continue to be resilient, flexible, and kind.
From risk to recovery and resilience
The COVID-19 pandemic is characterized by uncertainty and the future is unknown. These uncertainties, however, do not mean that recovery planning is not timely and essential. These uncertainties do mean that our planning must be based on best available information, adaptable, and contingent on local needs. While Public Health efforts to mitigate the effects of COVID-19 will continue, we will concurrently resume programs and services to address priority needs. By prioritizing recovery activities and reducing the growing backlog of services and unmet needs, Public Health Sudbury & Districts is an active partner in the local recovery endeavour—creating and contributing to post-pandemic strong and resilient communities.
End Notes
- Public Health Ontario. (2021, December 31). COVID-19 variant of concern Omicron (B.1.1.529): Risk assessment, December 29, 2021. https://www.publichealthontario.ca/- /media/documents/ncov/voc/2022/01/covid-19-omicron-b11529-risk-assessment-dec -29.pdf?sc_lang=en
- Public Health Ontario. (2022). Early estimates of Omicron severity in Ontario based on a matched cohort study of cases occurring between November 22 and December 24, Queen’s Printer of Ontario. https://www.publichealthontario.ca/-/media/Documents/nCoV/epi/covid-19-epi-enhanced-estimates-omicron-severity-study.pdf?sc_lang=en
- Bambra, C., Riordan, R., Ford, J., Matthews, F. (2020). The COVID-19 pandemic and health inequalities. J Epidemiol Community Health, 74(11), 964-968. doi:10.1136/jech-2020-214401.
- Bryant, T., Aquanno, S., & Raphael, D. (2020). Unequal impact of COVID-19: emergency neoliberalism and welfare policy in Canada. Critical Studies: An International and Interdisciplinary Journal, 15(1), 22-39.
- Ontario Ministry of Health, Ministry of Long-Term Care. (2021). Ontario Public Health Standards: Requirements for Programs, Services and Accountability – Protecting and Promoting the Health of Ontarians. Queen’s Printer of Ontario. Ontario Public Health Standards – Programs and Services – Health Care Professionals – MOHLTC (gov.on.ca)
- alPHa (Association of Local Public Health Agencies). (January 2022). Public Health Resilience in Ontario: Clearing the backlog, resuming routine programs, and maintaining an effective COVID-19 response. https://www.alphaweb.org/resource/collection/822EC60D-0D03-413E-B590-AFE1AA8620A9/alPHa_PH_Resilience_Report_Final_Jan2022.pdf
This item was last modified on February 17, 2022
